
Understanding Bipolar Disorder
What Is Bipolar Disorder?
Bipolar disorder is a chronic mental health condition that affects mood stability, often causing subtle to intense shifts between energetic highs (mania) and lows (depression).
Around 1 in 100 Australians experience bipolar disorder each year, with symptoms frequently emerging in the teenage years or early adulthood. Historically referred to as manic depression, “bipolar disorder” better captures the spectrum of mood episodes that people may experience.
Mood Episodes In Bipolar Disorder
In Bipolar Disorder, the experience of mania and depression may impact people differently, with episodes that can vary significantly in intensity and duration. Here’s a closer look:
Manic Episodes
During a manic episode, a person may feel unusually euphoric or agitated, energised, and confident, often leading to impulsive behaviors or even delusional thinking. They may experience psychosis where they see or hear things that aren't real, be more goal directed take on ambitious projects, speak rapidly, and struggle to sleep. These symptoms can significantly disrupt relationships, work, and even physical health.
Hypomanic Episodes
Hypomania, a milder form of mania, brings similar, but less intense, symptoms and is generally shorter-lasting. People in a hypomanic state may experience increased energy and productivity but are less likely to see their work or relationships disrupted. Even so, hypomanic episodes can be precursors to full manic or depressive episodes.
Depressive Episodes
Bipolar depression, is characterised by a low energy state, feelings of sadness, hopelessness, and exhaustion. During a depressive episode, individuals often struggle with daily functioning, start to isolate, and lack motivation, energy, or joy. These episodes can also impair one’s ability to work or engage in relationships.
Mixed Episodes
A mixed episode is characterised by the simultaneous presence of symptoms of mania, hypomania and depression. Individuals may experience heightened energy, restlessness, and racing thoughts while also feeling deep sadness, hopelessness, and irritability. These episodes can lead to significant distress and impaired functioning.
The frequency and duration of these episodes can vary widely. A person might experience episodes that last a few weeks, or symptoms that persist over several months. Importantly, these shifts in mood often appear disconnected from external events, leading to confusion and a sense of unpredictability for both those affected and their loved ones.
Bipolar Disorder Symptoms
A person with bipolar disorder goes through mood changes that range between manic, euthymic and depressive episodes.
Mania
Depression
Mixed Episode
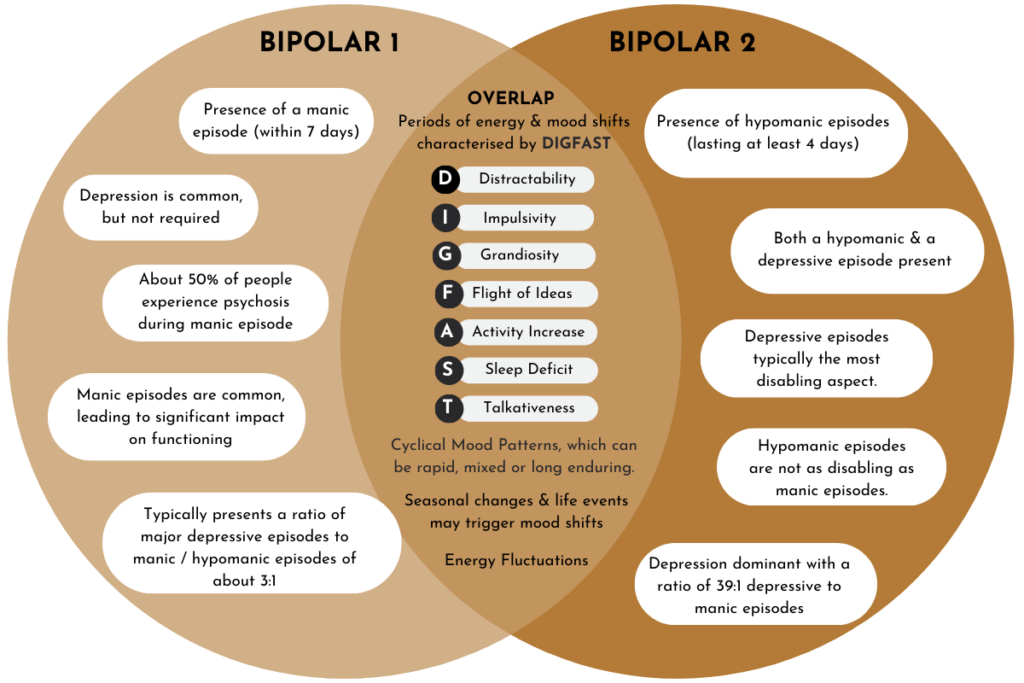
What are the types of Bipolar Disorder?
Bipolar disorder includes several subtypes, each with unique characteristics, and it exists on a spectrum of mood symptoms, ranging from mild to severe. Here’s an overview of the main types:
Bipolar I Disorder
This type involves manic episodes, where energy levels are so high that they can cause risky behavior, difficulty sleeping, and even impaired judgment. Manic episodes may last for at least a week and often require hospitalisation or lead to a break from reality (known as psychosis).
Bipolar II Disorder
With Bipolar II, the highs are less intense, called hypomania, but depressive episodes are more frequent and longer-lasting. Hypomania involves elevated mood or energy, but it’s not as severe as mania, so it often goes unnoticed or mistaken for normal excitement or personality trait. As a result health professionals can often misdiagnose this type for depression.
Cyclothymic Disorder
Cyclothymia is a milder form of bipolar disorder, with individuals experiencing hypomanic and depressive symptoms that are less severe and do not fully meet the diagnostic criteria for hypomanic or major depressive episodes. These mood fluctuations occur frequently and may persist for two years or more. Cyclothymia often leads to chronic mood instability but less functional impairment than Bipolar I or II.
Bipolar Spectrum Disorder
The bipolar spectrum includes individuals whose symptoms don’t fully meet the criteria for Bipolar I or II, often referred to as “soft bipolar.” These individuals may experience milder mania (hypomania), rapid cycling, or mixed symptoms that blur the line between mania and depression. Unlike Bipolar I and II, which have distinct manic and depressive episodes, the bipolar spectrum accounts for a wider range of mood and energy fluctuations that might not fit conventional diagnostic categories.
Together, these types and the broader bipolar spectrum specifier highlight the complexity and variety within bipolar disorder. Recognising these differences helps to tailor treatments to meet the unique needs of each individual, from managing full-blown mania to addressing milder mood fluctuations.
What causes Bipolar Disorder?
Bipolar disorder is a complex condition with various causes that are not entirely understood, but it is thought to arise from a combination of genetic, biological, and environmental factors:
Genetic Factors
In addition to family history, specific genetic variations have been identified that may contribute to an individual's susceptibility to bipolar disorder. Research suggests that genes involved in the regulation of neurotransmitters and brain function may play a key role in the development of the condition.
Thyroid Function
Thyroid dysfunction, particularly hypothyroidism or hyperthyroidism, has been linked to mood disorders, including bipolar disorder. Imbalances in thyroid hormones can affect neurotransmitter regulation and brain function, potentially triggering or exacerbating mood episodes such as mania or depression.
Circadian Rhythms
Circadian rhythm functions, which regulate the body's internal clock, have been shown to be more dysregulated leading to dysregulated mood episodes in bipolar disorder. These disruptions can lead to abnormalities in sleep-wake cycles, contributing to the onset or worsening of manic and depressive episode.
Metabolic Theory
In bipolar disorder, the energy-producing parts of cells, called mitochondria, may not work as efficiently as they should. This can lead to inflammation in the brain, which may disrupt mood regulation and how the body processes glucose.
These causes interact uniquely in each person, and understanding the complex interplay between genetics, biology, and environmental influences is essential for creating effective, individualised treatment approaches for bipolar disorder.
How is Bipolar Disorder diagnosed?
Diagnosing bipolar disorder is a detailed process conducted by a clinical interview. It typically involves an extensive assessment of the your symptoms, medical history, family history, and daily functioning. Diagnosis aims to differentiate bipolar disorder from other mood disorders and identify the specific type of bipolar disorder you may have to ensure appropriate treatment.
Clinical Interviews and Symptom Assessment
The first step in diagnosing bipolar disorder involves structured clinical interviews and discussion, where we explore your history of mood episodes, symptoms, and behaviors. In particular we look for episodes of mania or hypomania (e.g., elevated mood, increased activity, reduced need for sleep) and depression (e.g., sadness, fatigue, changes in sleep or appetite). By evaluating the frequency, duration, and impact of these episodes, we can assess how much symptoms interfere with your daily life and overall mental health.
Criteria from the DSM-5
Psychologists and psychiatrists use the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to determine if the individual meets criteria for bipolar disorder. The DSM-5 categorises bipolar disorder into types based on the nature of mood episodes
Psychological and Medical History
Reviewing your family history of mental health conditions is essential, as bipolar disorder has a genetic component. We may also assess medical factors, as thyroid disorders and information on your lifestyle, past trauma, substance use, and major life changes is also considered to identify potential triggers and plan treatment.
Differential Diagnosis
Since bipolar symptoms can resemble those of other conditions, such as major depressive disorder, borderline personality disorder, or ADHD, we will discuss these differences as well as review any co-occurring disorders, such as anxiety or substance use disorders.
Assessment Tools and Questionnaires
We may use assessment tools, like the Mood Disorder Questionnaire (MDQ) or Bipolar Spectrum Diagnostic Scale (BSDS). These can help evaluate symptoms and give insight into the severity and type of mood episodes. After gathering this comprehensive information, together we can arrive at a diagnosis and discuss treatment options, typically involving a combination of medication, psychotherapy, lifestyle changes, and psychoeducation tailored to your needs.
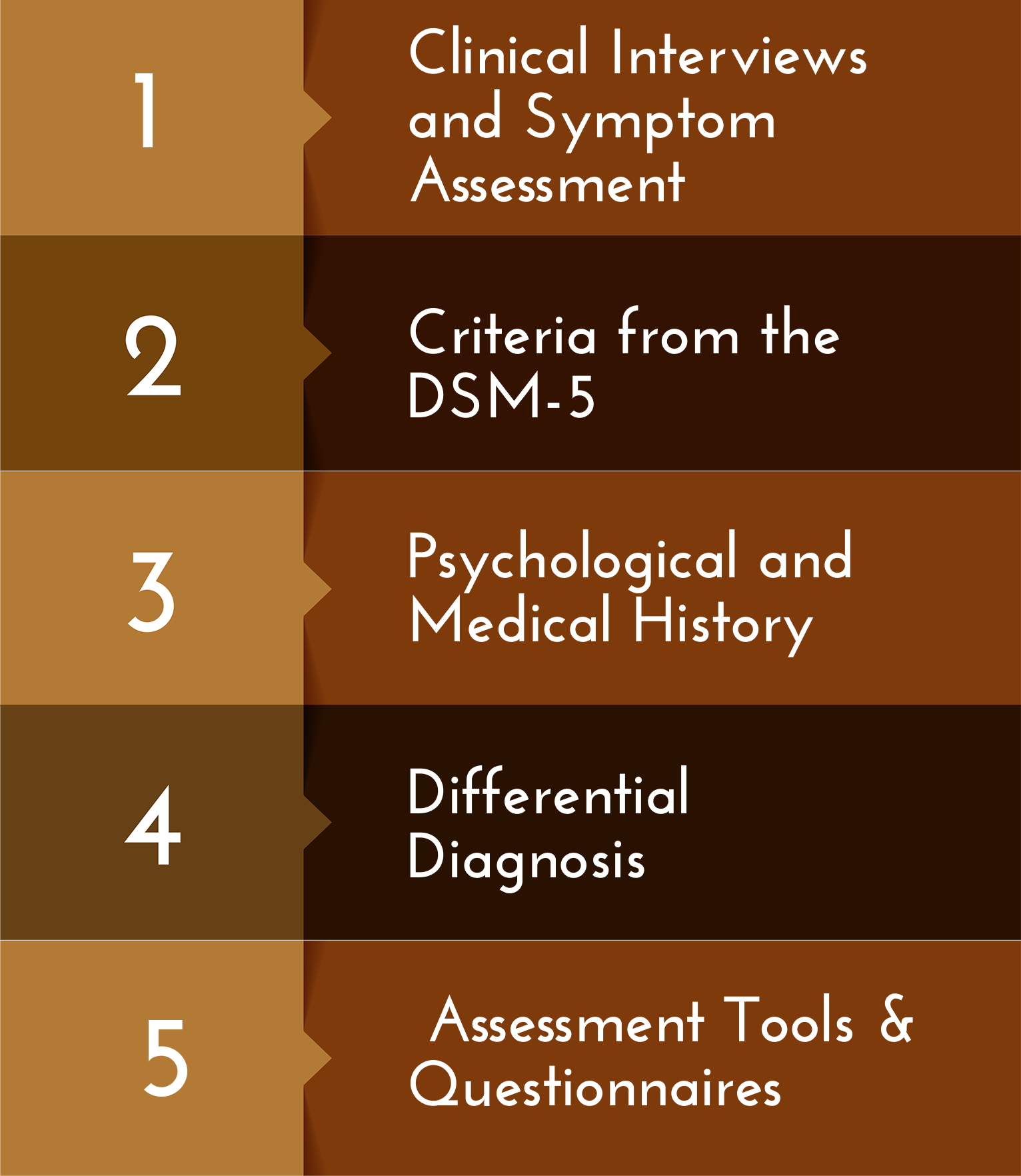
After gathering this comprehensive information, together we can arrive at a diagnosis and discuss treatment options, typically involving a combination of medication, psychotherapy, lifestyle changes, and psychoeducation tailored to your needs.

Ready to Take the Next Step?
If you’re experiencing mood swings or have been diagnosed with bipolar disorder, I can help. Book a session with me today to receive a thorough bipolar assessment and explore treatment options that can help improve your quality of life.